Evidence based research in nursing
Homeabout ojinfaqsauthor guidelinesfeatured authorseditorial staff boardcontact ussite 's newnew postingsjournal recognitionojin newsjournal topicsback to class: perspectives on school nursinghealthcare reform: nurses impact policyemerging global health concerns: how nurses respondelimination of barriers to rn scope of practice: opportunities and challengesorganizational outcomes for providers and patientsthe patient experiencecare coordinationcornerstone documents in healthcareemotional health: strategies for nursesmore... To the editorcontinuing edana is a peer-reviewed, online publication that addresses current topics affecting nursing practice, research, education, and the wider health care out more... Periodicalsojintable of contentsvol 18 2013no2 may 2013impact of evidence-based impact of evidence-based practice in nursing and the next big en r. Stevens, edd, rn, anef, impact of evidence-based practice (ebp) has echoed across nursing practice, education, and science. The call for evidence-based quality improvement and healthcare transformation underscores the need for redesigning care that is effective, safe, and efficient. Such initiatives include practice adoption; education and curricular realignment; model and theory development; scientific engagement in the new fields of research; and development of a national research network to study improvement. This article briefly describes the ebp movement and considers some of the impact of ebp on nursing practice, models and frameworks, education, and research. The article concludes with discussion of the next big ideas in ebp, based on two federal initiatives, and considers opportunities and challenges as ebp continues to support other exciting new thinking in on: stevens, k. May 31, 2013) "the impact of evidence-based practice in nursing and the next big ideas" ojin: the online journal of issues in nursing vol. Words: ebp, quality improvement, education, research network, translational science, institute of the past decade, nurses have been part of a movement that reflects perhaps more change than any two decades combined. The recommendation that nurses lead interprofessional teams in improving delivery systems and care brings to the fore the necessity for new competencies, beyond evidence-based practice, that are requisite as nurses transform healthcare. The recently-articulated vision for the future of nursing in the future of nursing report (iom, 2011a) focuses on the convergence of knowledge, quality, and new functions in nursing. The recommendation that nurses lead interprofessional teams in improving delivery systems and care brings to the fore the necessity for new competencies, beyond evidence-based practice (ebp), that are requisite as nurses transform healthcare. These competencies focus on utilizing knowledge in clinical decision making and producing research evidence on interventions that promote uptake and use by individual providers and groups of discussion highlights some of the responses and initiatives that those in the profession of nursing have taken to maximize the valuable contributions that nurses have made, can make, and will make, to deliver on the promise of ebp. A number of selected influences of evidence-based practice trends on nursing and nursing care quality are explored as well as thoughts about the “next big ideas” for moving nursing and healthcare is aimed at hardwiring current knowledge into common care decisions to improve care processes and patient ce-based practice holds great promise for... The chasm between what we know to be effective healthcare and what was practiced was to be crossed by using evidence to inform best ce-based practice holds great promise for moving care to a high level of likelihood for producing the intended health outcome.
Phrases in this definition bring into focus three aspects of quality: services (interventions), targeted health outcomes, and consistency with current knowledge (research evidence). It expresses an underlying belief that research produces the most reliable knowledge about the likelihood that a given strategy will change a patient's current health status into desired outcomes. 1) and urged all health professions to join efforts for healthcare pment of evidence-based practice is fueled by the increasing public and professional demand for accountability in safety and quality improvement in health care. Experts continue to generate direction-setting iom chasm reports (iom, 2003; iom, 2008a; iom, 2008b; iom, 2011a); each report consistently identifies evidence-based practice (ebp) as crucial in closing the quality chasm. The intended effect of ebp is to standardize healthcare practices to science and best evidence and to reduce illogical variation in care, which is known to produce unpredictable health outcomes. Development of evidence-based practice is fueled by the increasing public and professional demand for accountability in safety and quality improvement in health s in the field have defined ebp as “integration of best research evidence with clinical expertise and patient values” (sackett et al, 2000, p. Therefore, ebp unifies research evidence with clinical expertise and encourages individualization of care through inclusion of patient preferences. While this early definition of ebp has been paraphrased and sometimes distorted, the original version remains most useful and is easily applied in nursing, successfully aligning nursing with the broader field of ebp. The ebp process has been highly applied, going beyond any applied research efforts previously made in healthcare and nursing. This characteristic of ebp brought with it other shifts in the research-to-practice effort, including new evidence forms (systematic reviews), new roles (knowledge brokers and transformers), new teams (interprofessional, frontline, mid- and upper-management), new practice cultures (just culture, healthcare learning organizations), and new fields of science to build the “evidence on evidence-based practice” (shojania & grimshaw, 2005). This shift was apparent in the way nurses began to think about research results, the way nurses framed the context for improvement, and the way nurses employed change to transform on nursing this wide-ranging effort, another significant player was added…the policymaker. For example, through the magnet recognition program® the profession of nursing has been a leader in catalyzing adoption of ebp and using it as a marker of excellence. The evidence-based program, team strategies and tools to enhance performance and patient safety (teamstepps®) (ahrq, 2008) carries with it proven effectiveness of reducing patient safety issues and the program is available with highly-developed training and learning materials. Yet, because of the change necessary to fully implement and sustain the program across the system supported by organizational culture, a sophisticated implementation plan is required before the evidence-based intervention is adopted across an institution. While agency policy may be set, implementation and sustainment of teamstepps® remain on nursing models and in the ebp movement, nurse scientists developed models to organize our thinking about ebp. These frameworks guide the design and implementation of approaches intended to strengthen evidence-based decision making.

Once analyzed, these models can be grouped into four thematic areas: (1) ebp, research utilization, and knowledge transformation processes; (2) strategic/ organizational change theory to promote uptake and adoption of new knowledge; and (3) knowledge exchange and synthesis for application and inquiry (mitchell, fisher, hastings, silverman, & wallen, 2010). Listed among models in category 1 is the ace star model of knowledge transformation (stevens, 2004); this model is the exemplar for the present discussion of the impact of ebp on nursing models and ace star model of knowledge transformation (stevens, 2004) was developed to offer a simple yet comprehensive approach to translate evidence into practice. As explained in the ace star model, one approach to understanding the use of ebp in nursing is to consider the nature of knowledge and knowledge transformation necessary for utility and relevance in clinical decision making. Rather than having clinicians submersed in the volume of research reports, a more efficient approach is for the clinician to access a summary of all that is known on the topic. Likewise, rather than requiring frontline providers to master the technical expertise needed in scientific critique, their point-of-care decisions would be better supported by evidence-based recommendations in the form of clinical practice ace star model of knowledge transformation highlights barriers encountered when moving evidence into practice and designates solutions grounded in ebp. The ace star model emphasizes crucial steps to convert one form of knowledge to the next and incorporate best research evidence with clinical expertise and patient preferences thereby achieving ebp. Depicted in figure 1, the model is a five-point star, defining the following forms of knowledge: point 1 discovery, representing primary research studies; point 2 evidence summary, which is the synthesis of all available knowledge compiled into a single harmonious statement, such as a systematic review; point 3 translation into action, often referred to as evidence-based clinical practice guidelines, combining the evidential base and expertise to extend recommendations; point 4 integration into practice is evidence-in-action, in which practice is aligned to reflect best evidence; and point 5 evaluation, which is an inclusive view of the impact that the evidence-based practice has on patient health outcomes; satisfaction; efficacy and efficiency of care; and health 1. As an important new form of knowledge, systematic reviews are characterized as the central link between research and clinical decision making (iom, 2008). Resources for forms of knowledge in the star ption of graphic databases such as cinahl-provide single research reports, in most cases, multiple 2-evidence 3-translation into al guidelines clearinghouse-sponsored by ahrq, provides online access to evidence-based clinical practice guidelines. See 4-integration into 5-evaluation of process and on nursing ing the influential crossing the quality chasm report (iom, 2001), experts emphasized that the preparation of health professionals was crucial to bridging the chasm (iom, 2003). Programs for basic preparation of health professionals were to undergo curriculum revision in order to focus on evidence-based quality improvement processes. Leaders in all health disciplines were urged to come together in an effort for clinical education reform that addresses five core competencies essential in bridging the quality chasm: all health professionals should be educated to deliver patient-centered care as members of an interdisciplinary team emphasizing evidence-based practice, quality improvement approaches, and informatics (iom, 2003). Core competencies for health e patient-centered care - identify, respect, and care about patients’ differences, values, preferences, and expressed needs; relieve pain and suffering; coordinate continuous care; listen to, clearly inform, communicate with, and educate patients; share decision making and management; and continuously advocate disease prevention, wellness, and promotion of healthy lifestyles, including a focus on population in interdisciplinary teams - cooperate, collaborate, communicate, and integrate care in teams to ensure that care is continuous and evidence-based practice - integrate best research with clinical expertise and patient values for optimum care, and participate in learning and research activities to the extent quality improvement - identify errors and hazards in care; understand and implement basic safety design principles, such as standardization and simplification; continually understand and measure quality of care in terms of structure, process, and outcomes in relation to patient and community needs; and design and test interventions to change processes and systems of care, with the objective of improving e informatics - communicate, manage knowledge, mitigate error, and support decision making using information : iom health professions education, 2003, p. With a focus on employing evidence-based practice, nurses established national consensus on competencies for ebp in nursing in 2004 and extended these in 2009 (stevens, 2009). Through multiple iterations, an expert panel generated, validated, and endorsed competency statements to guide education programs at the basic (associate and undergraduate), intermediate (masters), and doctoral (advanced) levels in nursing. Between 10 and 32 specific competencies are enumerated for each of four levels of nursing education which were published in essential competencies for ebp in nursing (stevens, 2009).

These competencies address fundamental skills of knowledge management, accountability for scientific basis of nursing practice; organizational and policy change; and development of scientific underpinnings for ebp (stevens, 2009). Initiatives that followed included the new program standards established by the american association of colleges of nursing, crossing undergraduate, masters, and doctoral levels of education (aacn, 2013). The aacn standards underscored the necessity for nurses to focus on the systems of care as well on the evidence for clinical decisions. This systems thinking is crucial to effect the changes that are part of employing r curricular initiative became known as quality and safety education in nursing institute (qsen) (qsen institute, 2013). This close alignment reflects the appreciation that nursing must be part of this solution to effect the desired changes; and remaining in the mainstream with other health professions rather than splintering providers into discipline-centric on nursing t fields are emerging to understand how to increase effectiveness, efficiency, safety, and timeliness of healthcare; how to improve health service delivery systems; and how to spur performance improvement. Never before in healthcare history has the focus and formalization of moving evidence-into-practice been as sharp as is seen in today’s research on healthcare transformation efforts. These emerging fields include translational and improvement science, implementation research, and health delivery systems igation into uptake of evidence-based practice is one of the fields that has deeply affected the paradigm shift and is woven into each of the other fields. Several notable federal grant programs have evolved to foster research that produces the evidential foundation for effective strategies in employing ebp. Among the new research initiatives are the clinical translational science awards and the patient-centered outcomes al and translational science the public cry for improved care escalated, rapid movement of results into care was brought into sharper focus in healthcare research. The national institutes of health (nih), including the national institute for nursing research (ninr), developed the clinical translational science award (ctsa) program to speed research-to-practice by redesigning the way healthcare research is conducted (zerhouni, 2005). The term, translational science, was coined, and the definition was provided by nih (2010): “translational research includes two areas of translation. One [“t1”] is the process of applying discoveries generated during research in the laboratory, and in preclinical studies, to the development of trials and studies in humans. The second area of translation [“t2”] concerns research aimed at enhancing the adoption of best practices in the community. Nurse scientists have been significant leaders in the ctsa program, conducting translational research across these two areas. As part of the ctsas, nurse scientists conduct basic research and applied research, adding significantly to the interprofessional perspectives of the science. In relation to ebp, nurses are valued contributors to the “t2” end of the continuum of translational science, applying skills in mixed methods and systems t-centered outcomes evidence mounted on standard medical metrics...

Another recent and swooping change in healthcare research emerged with a focus on patient-centered outcomes research (pcor). As evidence mounted on standard medical metrics (mortality and morbidity), it was noted that metrics and outcomes of particular interest to patients and families (such as quality of life) were understudied. In 2010, attention was drawn to the need to produce evidence on patient-centered outcomes from the perspective of the patient. Congress founded and heavily funded the newly-formed patient-centered outcomes research institute (pcori) with the following mission: “the patient-centered outcomes research institute (pcori) helps people make informed health care decisions, and improves health care delivery and outcomes, by producing and promoting high integrity, evidence-based information that comes from research guided by patients, caregivers and the broader health care community” (pcori, 2013, para. Some of the most recent calls for research from the agency for healthcare research and quality (ahrq) are also focusing on pcor. These calls encourage early and meaningful engagement of patients and other stakeholders in stating the research question, conducting the study, and interpreting results (ahrq, 2013). This new direction in healthcare research will produce evidence that is co-investigated by patients and families in partnership with health scientists, increasing relevance so that ebp reflects the patient’s additional federal initiatives exemplify what may be called the next big ideas in ebp—each underscoring evidence-based quality improvement. Both initiatives emanate from the nih and both focus on generating evidence needed to make systems improvements and transform healthcare. The first is nih’s expansion of the program on dissemination and implementation (d&i) science; the second is the development of the research network, the improvement science research network (isrn). Call for increased emphasis on implementation of evidence-based practices brought forth a federal funding program. In this call for research proposals, implementation is defined as “the use of strategies to adopt and integrate evidence-based health interventions and change practice patterns within specific settings” (nih, 2013, section i, para 11). This research initiative will add to our understanding of how to create, evaluate, report, dissemination, and integrate evidence-based strategies to improve health (brownson, colditz, & proctor, 2012). Because of the central role that nurses play across all healthcare settings and clinical microsystems, research in this field is highly relevant to the profession. D&i research offers nurses opportunities to guide health care transformation at multiple levels, thereby addressing recommendation from the future of nursing. For example, one emphasis in the field is discovering and applying the evidence for the most effective ways to speed adoption of evidence-based guidelines across all health care professionals in the clinical unit and in the agency. Science research overriding goal of improvement science is to ensure that quality improvement efforts are based as much on evidence as the best practices they seek to implement.
As a new field, improvement science focuses on generating evidence about employing evidence-based practice, providing research evidence to guide management decisions in evidence-based quality improvement. The overriding goal of improvement science is to ensure that quality improvement efforts are based as much on evidence as the best practices they seek to izing that pockets of excellence in safety and effectiveness exist, there is concern that local cases of success in translating research into practice are often difficult to replicate or sustain over time. The isrn is an open research network for the study of improvement strategies in healthcare. The following shortcomings in research regarding improvement change strategies have been noted: studies do not yield generalizable information because they are performed in a single setting; the improvement intervention is inadequately described and impact imprecisely measures; information about sustainability of change is not produced; contexts of implementation are not accounted for; cost or value is not estimated; and such research is seldom systematically planned (iom, 2008b). Foundational to the network is the virtual collaboratory, fashioned to conduct multi-site studies and designed around interprofessional academic-practice partnerships in research. Isrn research priorities were developed via stakeholder and expert panel consensus and are organized into four broad categories: transitions in care; high performing clinical microsystems; evidence-based quality improvement; and organizational culture (isrn, 2010). The research collaboratory concept has proven its capacity to conduct multi-site studies and is open to any investigator or collaborator in the new nih d&i grant resources and the isrn collaboratory are “the next big ideas” in advancing ebp today. Story of ebp in nursing is now long, with many successes, contributors, leaders, scientists, and enthusiasts. From this admittedly selective overview of ebp, it is seen that the story of ebp in nursing is now long, with many successes, contributors, leaders, scientists, and enthusiasts. While there are benefits to both as the evidence is gathered and applied, the true benefit goes to the patient. As they emerge from formal education, students will see great enthusiasm for employing ebp in today’s clinical leading nursing science have access to new funding opportunities to develop innovative programs of research in evidence-based quality improvement, implementation of ebp, and the science of improvement. Readiness of the clinical setting for academic-practice research partnerships brings with it advantageous access to clinical populations and settings and an eagerness for utilization of the research challenges for moving ebp forward spring from two sources: nurses becoming powerful leaders in interprofessional groups and nurses becoming powerful influencers of change. Therefore, adopting the following habits hold promise for moving us ahead:Redesigning and/or investigating the redesign of healthcare systems through creativity and mastery of tence in educating the future workforce, and retooling the current workforce, with awareness, skills, and power to improve the systems of aside comfortable programs of research and picking up programs of systems ence on multiple perspectives and sound evidence for transforming nursing profession remains central to the interdisciplinary and discipline-specific changes necessary to achieve care that is effective, safe, and efficient. New in our vernacular and skill set are systems thinking, microsystems change, high reliability organizations, team-based care, transparency, innovation, translational and implementation science, and, yes, still evidence-based practice. Let us move swiftly to make these new ideas and skills ns of this work were supported by the national institutes of health, national institute of nursing research nih (1rc2 nr011946-01, pi k. Stevens is stti episteme laureate, professor and director of the academic center for evidence-based practice (ace) and improvement science research network (isrn) in the university of texas health science center school of nursing san antonio.

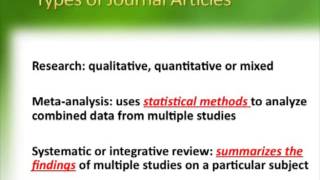
Her multi-site research on team collaboration and frontline engagement in quality improvement is conducted through the national collaboratory, the for healthcare research and quality (ahrq). The future of nursing: leading change, advancing health [prepared by robert wood johnson foundation committee initiative on the future of nursing]. Committee on standards for systematic reviews of comparative effective research; board on health care services]. San antonio, tx: academic center for evidence-based practice (ace) of university of texas health science center san s, k. O’keefe, phd, crnp; faye anderson, dns, rn, nea-bc (march 20, 2017)toward an understanding of wisdom in nursingsusan a. Matney, msn, rn-c, faan; kay avant, phd, rn, fni, faan; nancy staggers, phd, rn, faan (october 30, 2015)the value of library and information services in nursing and patient carejoanne gard marshall, phd, mls, mhs; jennifer morgan, phd; mary lou klem, phd mlis; cheryl thompson, msis; amber wells, ma (august 18, 2014)simulation in nursing practice: the impact on patient caremichelle aebersold, phd, rn; dana tschannen, phd, rn (may 31, 2013)hospital-based fall program measurement and improvement in high reliability organizationspatricia a. White, phd, rn, cphq, fnahq, nea-bc (may 31, 2013)the impact of emerging technology on nursing care: warp speed aheadcarol huston, msn, dpa, faan (may 31, 2013)nursing intellectual capital theory: implications for research and practicechristine l. Covell phd, rn; souraya sidani, phd (may 31, 2013)nursing control over practice and teamworkjessica castner, phd, rn, cen; diane j. For more information, please refer to our privacy > july/august 2014 - volume 12 - issue 4 > exploring evidence-based practice 's e-mail is name: (optional). You might appreciate this item(s) i saw at nursing made incredibly a copy to your message has been successfully sent to your error has occurred while processing your request. Please try after some noteprocitereference an, jolinda asn, rn; jordan, rita msn, rn; davis, charlotte bsn, rn, ccrn; williams, wanda msn, aprnnursing made incredibly easy! York va medical center in murfreesboro, authors have disclosed that they have no financial relationships related to this g where to types of quantitative types of qualitative an ebp n: permission ce-based practice (ebp) is the process of collecting, processing, and implementing research findings to improve clinical practice, the work environment, or patient outcomes. According to the american nurses association (ana), nursing interventions should be practical, methodical decisions based on ebp research studies. Utilizing the ebp approach to nursing practice helps us provide the highest quality and most cost-efficient patient care possible. Here we'll discuss the key characteristics of ebp relating to nursing to top | article ing all disciplines, ebp is an approach to clinical practice that's been gaining ground since its formal introduction in 1992. Starting in medicine, it then spread to other fields, such as nursing, psychology, and education.

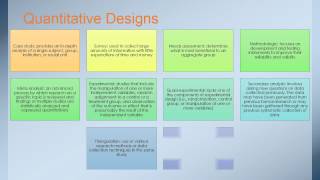
The ana predicts that by 2020, 90% of all nursing practice will be based on ebp research you incorporate up-to-date information from new ebp research, you'll be able to question current practices. You may ask questions such as, “are my current nursing interventions the most effective or safest for my patients? Nurses committed to ebp will compare current professional and clinical practices with new research facts and outcomes as they meet the 2020 goal, nurses must become proficient in evaluating various types of ebp research because they provide effective, proven rationales for nursing actions (see learn the lingo! Share these discoveries with your healthcare team to improve the essential components of your role and work to top | article g where to can find ebp research published in scholarly single-blind or double-blind peer-reviewed journals. The national institute of nursing research is well-known for comprehensive research studies that build the scientific foundation of our nursing practices; enhance hospice and palliative care; and help guide the prevention, treatment, and innovative management of universities, colleges, and formal nursing programs also conduct and publish research findings in their newsletters or scholarly journals, or on their websites. Remember to look for the latest research findings relevant to your job er obtaining appropriate institutional approval and conducting a formal research project of your own if you identify areas for improvement within your job role or work environment (see caution: permission required). Ebp research can be conducted in any area of nursing, including hospice care, geriatric or long-term care settings, in-patient hospital units, home care, substance abuse programs, and risk management. Besides improving patient outcomes and the work environment, research can help you evaluate social interactions, improve patient safety, resolve environmental issues affecting health, enhance quality of life, develop theories, explore healthcare economic issues, and address benchmarking needs or to top | article evaluating ebp nursing research studies, focus on these four criteria:* validity—the legitimacy, accuracy, and soundness of all aspects of the study. Failure to utilize ebp to guide nursing care increases the risk of poor to top | article tative and qualitative research are the two types of ebp research that nurses perform, evaluate, and utilize to guide nursing interventions and improve patient care (see quantitative versus qualitative research). When a research project utilized both quantitative and qualitative data, it's commonly called a mixed–methods research to top | article types of quantitative tative research consists of information expressed in numbers, variables, and percentages. This type of research focuses on specific, narrow questions in a double-blind study, usually with a large random group and variables. The data collected can be analyzed with the help of statistics in an unbiased manner with the objective to explain, describe, or tative research contains the following elements:* a random or specific study group with a common similarity. Variables (any element or behavior that can affect or change the outcomes of a study, such as a medication, treatment, or nursing intervention). Research is usually conducted in a controlled environment, such as a lab or healthcare unit. Correlational research is the methodical investigation of relationships or interactions between two or more variables without determining the cause-and-effect relationship the variables may have on each other. It also evaluates the underlying cause of a problem and studies the effects of variables (such as a nursing intervention) to evaluate their effect on the problem.

Descriptive research offers an accurate representation of the characteristics of a particular individual, situation, or group. Descriptive research is a way of discovering new meaning, describing numerically something that currently exists, determining the frequency with which something occurs, and categorizing to top | article types of qualitative goal of qualitative research is to generate new insight or knowledge, or to validate existing knowledge. This type of research focuses on systems, steps, rituals, processes, best practices, observations, or personal experiences, and may or may not have an outcome. Qualitative research can be used to gain a better understanding of a topic, inform the reader about how to perform a task, or gain a new perspective on a topic. It's helpful to explain sensitive, unique, and difficult-to-understand information that can't be conveyed ative research may consist of the following elements:Table quantitative v... The research may have a specific or global focus; for example, the group's interaction among themselves or with others, or social norms or taboos. This type of research reflects the theory that people behave or react in response to what they believe is true or correct, and not just based on what's objectively true. Historical research involves understanding and gathering information on the history of a topic, group, or culture. This type of research allows the reader to systematically evaluate historical information via a detailed analysis of past occurrences and guides the reader to what's been proven to be beneficial or ineffective in certain situations in the past. An example of this type of research is florence nightingale's discovery that unsanitary wound care and infrequent hand washing led to poor patient outcomes and that sanitary wound care with good hand washing improved patient outcomes. With this type of research, the investigator attempts to describe or understand a person's or group's perception, perspective, and understanding of a phenomenon and tries to answer the question, “what's it like to experience a given situation? By looking at multiple perspectives on the same situation, a researcher can make generalizations about what something is like from an insider's point of view. This research is typically focused on specific topics, such as a patient's response to illness, physical disability, healthcare procedures, or healthcare work to top | article an ebp age your healthcare team members to utilize and participate in ebp research studies when opportunities arise. Engage your colleagues and educate them on new ebp practices, studies, or interventions that may benefit their work environment or to top | article n: permission 't approach patients, families, or coworkers about participating in a research study until you've provided your healthcare facility with a clear research plan, including a hypothesis, objectives, and known variables. After presenting the research plan, obtain permission according to your healthcare facility's proceed with research, you must typically obtain permission from your healthcare facility, governing bodies, management teams, ethical standards boards, patients, families, and coworkers, if applicable. Patients recruited for the research should be given full disclosure of all the known variables so they can make informed decisions that are consistent with their ethical values and 's important for all members of the research team to be socially and ethically considerate of all participants in a research study.

Never pressure, coerce, or exert direct or indirect pressure on any potential participant in a research to top | article ch studies often contain language that may be unfamiliar to nurses. You can easily learn the basic lingo that's commonly found in research studies, such as:* abstract: a brief summary or overview of the research study. Control group: randomly selected participants from the research group who won't receive the experimental treatment or variable. Double-blind study: a research study conducted in which neither the investigators nor the participants know specific details of the study, such as whether a placebo or trial medication is being administered. Experimental research group: randomly selected participants from the research group who will receive the experimental treatment, medication, or variable. Single-blind study: a research study conducted in which the investigators know specific details of the study but the participants don't. Variable: an intervention, action, or medication that's being studied to observe its effect on the research group. In this scenario, the new medication is the intervention or to top | article conducting research, think fy common (pick a specific research design). Pertinent data such as past medical icate your research goals with the healthcare with the research study participants (goals, risks, and benefits). Your plan after you obtain the participants' written t the data and write your to top | article g where to types of quantitative types of qualitative an ebp n: permission ing evidence-based practice g made incredibly easy12(4):8-12, july/august 's e-mail is name: (optional). Patient safety and quality: an evidence-based handbook for detailshughes rg, lle (md): agency for healthcare research and quality (us); 2008 tssearch term < prevnext >. Sity of iowa hospitals and clinics, department of nursing services and patient careaddress correspondence to: marita g. University of iowa hospitals and clinics, department of nursing services and patient care, 200 hawkins drive rm t10 gh, iowa city, ia 52242-1009. Chapter version of this page (470k)in this pagebackgroundresearch evidencepractice implications from translation scienceconclusionsearch strategyreferencesother titles in this collectionadvances in patient safetyrelated informationpmcpubmed central citationspubmedlinks to pubmedsimilar articles in pubmedthe effectiveness of integrated care pathways for adults and children in health care settings: a systematic review. The effect of a translating research into practice intervention to promote use of evidence-based fall prevention interventions in hospitalized adults: a prospective pre-post implementation study in the u. 2016]the effect of a translating research into practice intervention to promote use of evidence-based fall prevention interventions in hospitalized adults: a prospective pre-post implementation study in the mg, conlon p, reynolds ma, ripley r, tsodikov a, wilson ds, montie m.

Evidence for evidence-based practice implementation - patient safety and qualityyour browsing activity is ty recording is turned recording back onsee more...
