Privacy in research ethics
It should be read by those looking for both a fundamental and thorough understanding of privacy and confidentiality issues. Reporting breaches of confidentiality to the irb and the privacy officer/gh this resource will be helpful in understanding privacy and confidentiality issues in research, it should not be considered legal advice. Viewing this web-based educational program should not substitute for reading the full text of the privacy rule, as this program covers only a select few of the hipaa note that many of the links provided are not maintained on, or affiliated with, columbia university servers. Our modern research setting, with growing dependence on computers, the internet, and the need for databases and registries, protection of an individual’s privacy is now one of the greatest challenges in the earliest days of medicine, the notion of privacy and confidentiality has been the cornerstone of the patient-physician relationship; more recently, it has become a crucial consideration in the research participant*–researcher relationship. Are now conducting more research in the behavioral sciences, the social sciences, economics, and psychology, resulting in increasing amounts of personal information being collected. A breach of confidentiality violates a person’s rights and poses a risk of dignitary harm to the research participant, ranging from social embarrassment and shame, to stigmatization, and even damage to social and economic status, such as loss of employment and health are many specific topics that fall under the rubric of privacy and confidentiality that are essential to consider by today’s researchers, institutional review board (irb) members, irb and institutional administrators, and institutional privacy officers/boards. This learning module includes a discussion of the health insurance portability and accountability act of 1996 (referred to as the hipaa privacy rule in this module) as it relates to research, yet our goal for this module is not to focus on the hipaa privacy rule but, rather, to increase awareness of how protecting privacy and maintaining confidentiality in the research setting have become ever more critical, complex, and y is defined in terms of a person having control over the extent, timing, and circumstances of sharing oneself (physically, behaviorally, or intellectually) with others. Privacy refers to the right of individuals to limit access by others to aspects of their person1 that can include thoughts, identifying information, and even information contained in bodily tissues and fluids. Even though privacy is not explicitly mentioned in the united states constitution, many consider privacy a basic human right and maintaining confidentiality a professional 1993, the council for international organizations of medical sciences (cioms) and the world health organization (who) published the ethical guidelines for biomedical research involving human subjects. These guidelines provide explicit provisions for respecting the privacy of research participants and maintaining the confidentiality of their personal information. It is important for researchers to understand how these competing values can be viewed and how to balance the researcher’s goals against these competing needs. As vulnerable populations, their concerns are important for the researcher to recognize and address as the legitimacy of a study is in jeopardy if potential participants are reluctant to reveal vital ts of maintaining confidentiality:It helps establish trust between the research participant and the reduces worry on the part of the maintains the participant’s participant feels gives the participant control and promotes individuals should risk harm due to disclosure of their private information as a result of their participation in research. A researcher's obligation to protect confidentiality is higher than a clinician’s since research often does not provide benefit to the participant and provides no compelling reason to become involved in the research. Those involved in designing, approving, and carrying out research must determine how to conduct research that maintains participants’ limited circumstances, personal information may be disclosed in the public interest without an individual’s consent when the benefits to society outweigh the individual’s interest in keeping the information confidential. Balancing societal interests in research must be carefully considered by the investigator and approved by the institutional review board (irb) and the privacy officer/board. Federal regulations, guidance, and belmont report (1979), written by the national commission for the protection of human subjects of biomedical and behavioral research, is the major ethical statement guiding human research in the united states and is the basis for u. Individual privacy and autonomy are described in the report as necessary to honor these ethical principles. 1 code of federal regulations title 45 part 46: the common 45, part 46 of the code of federal regulations (45 cfr 46) also known as the common rule, defines human subjects as living individuals about whom a researcher obtains:Data through intervention/interaction with the individual, fiable private common rule is clear that these data need to be protected. 7), "when appropriate, there are adequate provisions to protect the privacy of subjects and to maintain the confidentiality of data. 2 food and drug administration regulation: 21 food and drug administration (fda) requires statements in the informed consent form:That describe the extent to which confidentiality of records that can identify the participant in the research will be maintained, inform the participant that the fda may view the research records. Of confidentiality (cocs), issued by the national institutes of health (nih), allow the researcher to refuse to disclose identifying information on research participants in any civil, criminal, administrative, legislative, or other proceeding, whether at the federal, state, or local level, unless the participant researcher can apply to the nih for a certificate of confidentiality, whether or not the research is federally funded. Certificates of confidentiality are used when research information is considered sensitive and disclosure could have adverse consequences for participants or damage their financial standing, employability, insurability, or reputation. Researchers should consider applying for a certificate of confidentiality if their study involves genetics, hiv/aids, certain communicable diseases, including sexually transmitted diseases, substance abuse, mental illness, criminal behavior, and other stigmatizing illnesses and are, however, limitations to certificates of confidentiality. A researcher must disclose in the informed consent form any circumstances in which the researcher would need to disclose identifying information to departments of health or other authorities (e. Do not prohibit researchers from voluntarily disclosing identifying information they have ipants should also be informed that if they themselves reveal to others sensitive information, or the fact of their participation in the research study, the certificate of confidentiality is no longer chers can apply for a certificate of confidentiality only after irb approval of the research protocol. Some institutions withhold final irb approval for recruitment until the certificate of confidentiality is in application should be sent to the nih at least three months before the start of recruitment of research participants. If there are significant changes in the research protocol after irb approval, then an amended certificate must be applied for through the original nih institute granting the certificate. 4 hipaa privacy rule: relevance for : this module provides only a brief overview of the hipaa privacy rule.

See the federal government sources for a more complete privacy rule: information for privacy rule and its impacts on al research and the hipaa privacy y of the hipaa privacy consider consulting your local federally funded and some privately funded behavioral and biomedical research in the united states includes protections to help ensure the privacy of participants and the confidentiality of information through the u. The hipaa privacy rule supplements these protections by requiring covered entities to take specific measures to safeguard the privacy of individually identifiable protected health hipaa privacy rule regulations took effect april 14, 2003. They were the first comprehensive federal department of health and human services (dhhs) guidelines for the protection of the privacy of protected health information (phi). The hipaa privacy rule does not regulate researchers per se, but may affect their ability to access an individual’s protected health information for research and may require them to meet the conditions of the hipaa privacy rule by providing proper hipaa privacy rule allows a covered entity (e. A healthcare institution) to disclose protected health information for research under the following conditions:If research participants provide a written authorization (see section 2. Is important to keep in mind that medical records-based research, in which the protected health information comes from documents or databases, and not directly from participants, is also subject to the hipaa privacy record reviews preparatory to research, the researcher should provide the required documentation to the privacy officer/board (see section 2. Activities preparatory to are times when researchers need to review medical records in preparation for research. This could be:When information may be helpful in the preparation of a research hypothesis, a protocol itself, or a grant application, it is necessary to identify potential participants who meet the eligibility requirements of a study. Researcher is allowed to identify, but not contact, potential study participants under the preparatory to research provision. Before permitting this activity, a covered entity must receive the proper documentation from the researcher. No phi may be removed from the covered entity during this preparatory institutions may require all activities preparatory to research to be reported to and reviewed by the institution’s privacy officer/board. Approval under the hipaa privacy rule does not in any way affect the stipulations of 45 cfr 46 regulations. Recruitment: identifying and contacting research conducting a clinical trial, recruiting the appropriate participants is critical. Patients expect that information about their medical condition will be kept confidential and might consider it a breach of confidentiality if they were contacted by a researcher not involved with their primary physician should contact a patient (potential participant) first to get his or her permission to be contacted by the researcher. If the nature of a study makes this very difficult (impracticable), a researcher must provide reasons to the privacy officer/board that justify why such a procedure would not be practicable and obtain a waiver for recruitment. Problematic situation arises when personal information is collected while screening potential research participants who are later found, for one reason or another, to be ineligible to participate. In this instance, it is best to have explicit procedures outlined in the research protocol for securing or destroying the collected screening otherwise permitted by the hipaa privacy rule, a subsequent authorization must be obtained from the participant before a covered entity researcher may use or disclose the participant’s phi for the clinical trial 2003, the american association of medical colleges (aamc) conducted a survey of researchers, irb members, privacy officials, deans, and others. Some researchers have called for revisions of the hipaa privacy rule that would remove the barriers and burdens that the privacy rule has created for recruiting. Research participant must give specific written permission to a researcher to use the participant’s protected health information (phi). According to the hipaa privacy rule, the authorization for research applies to the specified research and not to any future unspecified projects. Transition provisions: research that started before april 14, research was ongoing or originated before the date hipaa went into effect—april 14, 2003—hipaa contains provisions that allow a researcher to use prior permissions obtained from a participant granted either by the participant through the informed consent process or by an irb a waiver of consent had been granted prior to april 14, 2003, but informed consent was or will be obtained after that date, then the participant’s authorization is required under hipaa unless a waiver of authorization is granted. Waiver of certain circumstances, it may be difficult for researchers to obtain a written authorization from research participants. Research conducted on existing databases or repositories in which no contact information may be available is a good example. To address these situations, the hipaa privacy rule contains criteria for the waiver or alteration of the authorization requirement by a privacy officer/board. The privacy officer/board can waive the requirement that the research participant needs to sign an authorization. This would be when:The research use of the health information does not represent more than a minimal risk to privacy;. Research could not be done without the requested health information; would be difficult to obtain signed authorizations from the research researchers receive phi under a waiver of authorization and subsequently disclose any of that information to other researchers, institutions, or agencies, the researchers become responsible for keeping an accounting of disclosures for phi. Under hipaa, research participants can request a record of how often their health information was released to others in the previous six-year period.

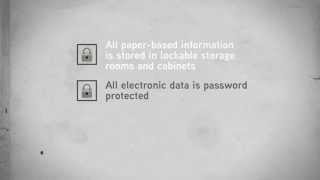
Protocol (ip) address ric identifiers, including finger and voice -face photographic images and any comparable other unique identifying number, characteristic, or code, unless otherwise permitted by the privacy rule for re-identification. The use of a limited data set allows a researcher and others to have access to dates of admission and discharge, birth and death, and five-digit zip codes or other geographic subdivisions other than street address. A limited data set does not include specified direct identifiers of the individual’s relatives, employers, or household use a limited data set, the researcher must sign a data use agreement that limits who can use or receive the limited data set. It requires that the researcher neither re-identify the data nor contact the research participant and contains assurances that appropriate safeguards will be used to prevent improper use or disclosure of the limited data set. Questions about the use or disclosure of hiv/aids data should be directed to an institution’s privacy officer/board. On the state where the research is conducted, waivers of authorization may not be permitted with fully identified hiv data. Decedent’s ch on decedent (deceased persons) information is still protected under the hipaa privacy rule even though it is not covered by the common rule regulations (45 cfb 46) and thus does not require irb approval. Check your institution’s use or disclose phi of deceased persons for research, covered entities are not required to obtain an authorization, a waiver, an alteration of the authorization, or a data use agreement from the personal representative or next of kin. However, the covered entity must obtain from the researcher who is seeking access to the decedents' phi:Oral or written representations that the use and disclosure is solely for research on the phi of decedents;. Or written representations that the phi is necessary for research purposes; ntation, at the request of the covered entity, of the death of the individuals whose phi is sought by the researcher. Public health surveillance research and sly, public health services provide important essential public health protections. The hipaa privacy rule permits the sharing of phi for public health purposes without individual authorization if the phi is provided to a legally authorized public health authority for the purpose of preventing and controlling disease, injury, or disability. It is generally accepted that adolescents’ concerns about protecting their privacy might prevent them from seeking medical treatments for certain conditions (e. Sexually transmitted diseases, substance abuse, and pregnancy) and might also prevent them from volunteering for important research studies. Researchers need to be aware of the impact of such regulations on protecting the confidentiality of research data for adolescents and the impact this has on their protocols, particularly when obtaining informed consent that involves parents or guardians. Data storage requires researchers to use secure procedures for all computer-based storage of protected health information including servers, laptops, handheld computers, and any other type of data storage ty procedures (e. Encryption, password protection) should be standard practice whenever conducting research using databases that include identifiers. Fines imposed for violation of ions of the hipaa privacy rule can result in both civil and criminal penalties, including fines and possible time in office of civil rights of the department of health and human services enforces civil violations. The hipaa privacy rule allows fines of up to $100 per person for each violation of the law, to a limit of $25,000 per year for violations of a single standard per calendar department of justice enforces criminal violations of the hipaa standards. Irbs’ role in protecting and privacy boards/officers, which may or may not be separate entities, depending on the institution, are designed to ensure that there are adequate provisions to protect the privacy of participants and to maintain the confidentiality of the ch participants must be given fair, clear, honest explanations of what will be done with information that has been gathered about them and the extent to which confidentiality of records will be maintained. Under court order or subpoena for example, there may be legal reasons for compelling a researcher to disclose the identity of, or information about, a research participant. In some instances, a researcher may be mandated to report information to government agencies as in cases of child abuse or elder abuse, certain communicable diseases, illegal drug use, and other situations such as gunshot chers are often unsure about what privacy protections to include in the informed consent form. Provide the following suggestions to irbs when reviewing protocols: the following: the sensitivity of the information, the length of time the information is being held, the usefulness of the information collected, and the ability to protect the research is conducted across multiple sites, review how the information is being protected. Make sure that duplicated information is properly destroyed when transferring confidentiality procedures during the continuing review of protocols by reexamining the protection of sensitive information and the success of the protection e researchers, research coordinators, and irb staff on data management and data perplexing for irbs and researchers are situations when it is not possible, or thought to be too difficult, to obtain a hipaa perplexing, are situations in which the irb must determine which safeguards should be in place to protect past participants who need to be contacted to sign a new informed consent form. The irb or privacy officer/board must review the researcher’s plan to deal with these situations and determine whether the privacy protections specified in the protocol adequately protect the participants. Data protection: protecting data is key to reducing studies require protecting privacy and maintaining confidentiality of data even if they are not covered under the hipaa privacy rule. Behavioral and social sciences research conducted at a university that is not a covered entity may not fall under the hipaa regulations. Such research would involve the hipaa privacy rule when disclosure from a covered entity is needed to conduct the ing study-specific protections for confidentiality requires planning, diligence, time, and knowledge of privacy and confidentiality strategies and procedures.

Researcher may opt to code information by replacing identifying information of the individual with a number, letter, symbol, or some combination. Generally researchers themselves should not be able to re-identify the data but might ask a third party to trace identifiers back to the individual. State-level hipaa privacy rule is not the only government regulation that pertains to the privacy of health information. Therefore, it is important to check state laws to determine whether the hipaa privacy rule or state privacy laws prevail. Generally, state laws that provide additional privacy protections in a specific area will supercede the hipaa regulations in those areas. State laws that require reporting of disease or injury, child abuse, elder abuse, birth, death, or public health surveillance, are not overridden by the privacy rule. 6: genetics research: the uniqueness of genetic are differences of opinion about the significance of genetic information for individuals and their families. Genetic information also can be revealed about individuals (and their families and populations) simply from a tissue sample or uently, the decoding of the human genome makes privacy and confidentiality issues extremely acute. Medical research centers and other health care organizations will need to revise current protection procedures to avoid dignitary harms, such as stigmatization and discrimination associated with violations of genetic results of genetic research even have the potential to stigmatize whole populations that share a common gene pool. This will present a significant challenge to protecting privacy and maintaining confidentiality in the collection and storage of dna samples for pharmacogenomic research. Genetic privacy of individuals and ipants often express anxiety and concern about privacy aspects of the informed consent process. Congress to pass a genetic information nondiscrimination chers interested in the possibility of studying genetic markers for diseases or treatments need to learn how to plan appropriately to collect data and how to contact participants for future research and follow-up. Are the obligations, if any, of the researcher to notify the proband’s (research participant’s) family members of their genetic risk? When a physician’s “duty to warn” is in conflict with his or her obligation to respect the privacy of patients, offit et al. Respectful in approaching people and eliciting medical histories and information about e in the informed consent form any possible commercial application resulting from their genetic material for which they will not realize any t the interlinking of databases that could reveal personal ish confidentiality and data security p measures to handle requests for personal data by public health authorities, police, courts, employers, lenders, insurers, and subjects' sound data access, ownership, and intellectual property clear about whether and how study participants will be informed of findings that might be medically helpful to e review and oversight by research ethics and privacy protection bodies. Genetic privacy and state l consideration of a state’s genetic privacy laws is called for when conducting genetic research. Many states have passed genetic privacy laws that provide protections in addition to the protections provided by federal privacy laws. Some states explicitly define genetic information as personal property; some consider dna samples as personal property, and some states have penalties for violating genetic privacy national conference of state legislatures publishes information on the specific laws passed by each addition, many states have passed genetic and health discrimination laws. Ethical issues in pedigree research are complicated because there can be potential conflicts between the rights and responsibilities of an individual and of a group. The privacy and autonomy of one family member can conflict with the privacy and autonomy of another individual or a ee research relies on an accurate determination of family history, therefore, it is important to get full family participation. There are strategies to protect identities in published pedigree diagrams such as omitting gender information in unaffected family members, collapsing unaffected children into a single icon, and including only a portion of the human genome research project will yield knowledge about disease prevention and treatments utilizing information about gene function. Finding the appropriate balance between privacy and genetic research should be continually considered as genomic medicine find the right balance between privacy and research, researchers and policymakers might consider anonymizing the data or permitting the use of protected health information in limited circumstances. 7: special considerations in the application of privacy and ic types of research can present unique challenges to protecting privacy and maintaining confidentiality. A brief review of some of these additional challenges is presented below to provide a more comprehensive picture of considerations needed to protect research participants. Researcher may be required to report protected health information to certain agencies and authorities, particularly to local and state agencies when required by judicial requests. Major risk in social sciences and behavioral research “is that of inadvertent disclosure—either during collection, processing, or storage of the original data, or through the identification of participants in data files that are made available for secondary analysis. 33 stigmatization of specific individuals or groups—for example, by ethnicity, mental health, medical diagnosis, family history, or substance abuse—is an important concern that requires extra assurances of and behavioral research may present dilemmas for researchers when data resulting from a behavioral study (such as the use of a personality scale or depression inventory) suggest that a participant might be at risk of harming himself or herself. There may be an obligation to provide ancillary care when certain diagnostic insights are realized during research.

The researcher should consider that participants entrust only specific aspects of their health to the researcher, not necessarily their health in general. The researcher should consider the scope of what is entrusted to him or her by the participants, and what is his or her duty to care for their well-being. 3 third party chers sometimes seek to obtain private and sensitive information about others who are not participants in the research. Especially in epidemiological studies, researchers often collect data from the proband (the affected individual who led to the research done on their family) about family members even though informed consent is provided only by the r, if the information collected about these “others,” is considered private and sensitive and these “others” are readily identifiable, these “others” can be considered third party research participants. In designing protocols, researchers must consider whether any third party may be adversely affected by the office for protection from research risks (oprr), now the office for human research protections (ohrp), closed down hundreds of research studies at virginia commonwealth university (vcu) in 1998 as a result of concerns about protections of privacy, informing the university, in the case of richard curtin, that the vcu researcher should have sought mr. However, it is important to remember that vulnerability may apply to populations that are otherwise not viewed as vulnerable but are considered vulnerable depending on the particular research ivity to being vulnerable is relative. African-americans are less trusting of medical research, given their fears of discrimination based in part on past experiences (e. In contrast, latinos may be overly trusting and assume that physicians conducting clinical research would not be “doing experiments” on them. Gay men and lesbians also may be particularly concerned about their privacy and wary of medical research. 37 research participants living with hiv, mental illness, or particular genetic disorders may also have specific concerns. Given this, many groups may require especially arduous consent procedures needing detailed chers and their staff need to be trained to be sensitive to the complexities and particular dilemmas potential participants face concerning privacy and disclosure and to communicate appropriately so participants can make informed decisions about volunteering for research. 5 couple and family and family research studies can be complicated because family members may confront competing interests. These studies require special attention to privacy and s of the same family from different generations may have different sensitivities to the same s and children may not have the same perspective on what the other views as sure of personal information from one participant may reveal information about other family research often requires family members to reveal private information about themselves that they would not ordinarily want to share with other family studies can pose risks to the family unit in addition to risks to the researcher needs to carefully consider what research data might be disclosed, to whom, and under what circumstances. Typically, standard ethical guidelines and federal regulations do not adequately address issues regarding disclosure of data involving the privacy of multiple family members. Therefore, researchers need to establish clear boundaries before the release of data from their research, and they should communicate these boundaries to all family important issue is whether researchers should share with parents information about their child. Family researchers should clearly specify their policy on the limits of confidentiality with minors and include those in both their consent and assent processes. Disclosure by adolescents about their use of drugs or alcohol, or about their suicidal ideation, could be motivated by a hope that the researcher will help them with their problem. Parents and adolescents prefer protocols that give permission to the researcher to obtain help if there is a serious problem such as drug use or suicidal behavior. Research in the increased concern regarding employee health and safety has resulted in an increase in studies conducted in the workplace. This leads to an often subtle vulnerability that can be easily discounted by the researcher. Neurogenetics) has created an increase in the amount of sensitive information collected that research participants might prefer to be kept private. However, he also counter-argues that providing special protections for neuroscience information may not always be necessary, since not all neuroscience information may prove to be meaningful or sensitive and may be hard to separate from other types of medical future of neuroscience research requires the vigilant monitoring of privacy and confidentiality implications to determine when situations provide acceptable privacy protections and when additional protections are necessary. Individuals might be linked to or identified with the community or a subgroup within the community, and may experience stereotyping, discrimination, or stigmatization simply by being identified as a member of that ore, as marshall states, “it is vitally important for researchers to work collaboratively with the study population to ensure those participants and the communities they represent are benefitted from and are empowered by the research, not devalued or harmed. 9 high-profile research: disclosure in the gh only a few research studies fall within this category, occasionally a high-profile clinical trial, one involving a new, dramatic, high risk, potentially life-saving technology, attracts avid media coverage. Morreim discussed the abiocor artificial heart trial as an example in which the company, abiomed, tried (unsuccessfully) to implement a limited information-dissemination policy designed to protect the privacy of the research participants as well as the research/clinical team. Morreim argued that researchers have an obligation to keep the public informed about such trials, but she also raised questions about what types of information belong, or do not belong, in the press. In some situations, hospital staff and administration may have to take forceful actions to protect privacy (e. 10 international research and disclosure would prevent serious harm to public health,By order of a court of law for a criminal countries, various international laws and regulations regarding privacy and confidentiality apply.

Tissue and data of privacy and confidentiality must be considered when biological materials or tissue samples used in research contain identifiers. Registries, banks, and libraries) are used for research, they must satisfy both the common rule (45 cfr 46) and the hipaa privacy , the proliferation of databases for all types of data collection, and the potential to network and link databases for a variety of purposes across academic, commercial, and public health research, require careful stewardship. Internet et research is an area replete with research ethics concerns that need to be addressed. Chat rooms, discussion boards) are fertile and invaluable sources of qualitative data uniquely accessible to researchers. Members of internet communities do not have the expectation to be research participants and may consider a researcher lurking around a self-help chat room to be a voyeur, taking advantage of people in distress. Their privacy can easily and unintentionally be violated by a researcher who quotes their exact words. Even if the researcher deletes all personal information, powerful search engines can index web pages so that the original message, including the email address of the sender, could be retrieved by anyone using the direct quote as a et-based research can be classified into three types: (1) passive analysis, when researchers gather information from discussion groups without identifying themselves; (2) active analysis, when researchers participate in the communications (they may or may not identify themselves as researchers); and (3) information analysis, when researchers identify themselves and gather information through online interviews or focus groups to recruit participants for other forms of approving internet research, eysenbach and till propose seven issues for researchers and irbs to consider and address, including (1) the extent of intrusiveness, (2) perceived privacy, (3) vulnerability, (4) potential harm, (5) informed consent, (6) confidentiality, and (7) property ic questions for researchers to consider when conducting internet-based research are:What are the risks of exposure of the research participant’s identity during data gathering, data dissemination, and publication? Researchers are using the internet to screen potential participants for study eligibility, recruit participants, and, transfer data. Researchers need to be aware of the potential ramifications of privacy breaches, the potential harms of such activities, and how to address them. As in all research involving identifiers, researchers need to develop “tight” security policies, such as increased password protections, encryption techniques, and firewalls on computers to obstruct outside hackers. 13 secondary collected for previous research and considered to be “on the shelf” at the time of the second study can provide very useful information that might be difficult and expensive to acquire otherwise. The privacy risks to these individuals must be weighed against the potential societal benefits from the research. Irbs need to exercise good judgment to determine whether a researcher conducting secondary research needs access to coded data or protected health information with ary use of data is allowed for the purpose of research, public health, or health care operations. Name, age, address, telephone, fax numbers, medical-record numbers, vehicle license-plate numbers, and fingerprints) must be redacted (edited to remove sensitive or confidential information) in order to safeguard the privacy of the the secondary data set contains no identifiers, then 45 cfr 46 may not apply. 14 public health surveillance ethicists and researchers have argued that in certain circumstances, privacy should be limited to enable appropriate and much needed public health surveillance. 59 ,60 others argue that medical information used for purposes of research without the knowledge or consent of the donor, often as part of national databases and biobanks, is and fairchild have called for some form of explicit, systematic, ethical review in public health surveillance, particularly since it is often difficult to distinguish between research and practice in certain public health surveillance efforts. In addition, discrepancies exist between state and federal definitions of what is practice and what is research, thereby making it difficult to determine the need for irb review. Bayer and fairchild believe the tensions between individual privacy interests and collective public health interests would be better served by some form of explicit systematic review in order to avoid breaches of confidentiality and stigmatizing events. Breach of confidentiality should be taken seriously by researchers and a plan of action should be implemented to rectify any breaches of confidentiality. A breach of confidentiality might be considered an adverse or unanticipated event by an irb, therefore, breaches need to be reported promptly to both the irb and the privacy officer/board. In addition, a review session with the privacy officer/board might be required and additional data protections, such as encryption, might be right of a research participant to privacy and to have his or her protected health information (phi) kept confidential is both respected and expected today. As research in science and medicine advances, particularly in the ever-expanding fields of genetics, neurosciences, and behavioral sciences, and as more phi is collected, protecting privacy and maintaining confidentiality are becoming increasingly complex and complicated educational module has touched on a variety of critical concerns for researchers to consider regarding protecting privacy and maintaining confidentiality. Researchers and irb members need to recognize the overt and covert threats to privacy that participants face, and use appropriate strategies to promote confidentiality. Consistent vigilance is required if researchers are to maintain the trust of the public that is so essential in the pursuit of knowledge designed to improve the health and welfare of ue to the next section:1 mccabe m. Comment from the conflicts of interest, privacy/confidentiality, and tissue repositories: protections, policies, and practical strategies conference co-sponsored by prim&r and the columbia university center for bioethics. The hipaa privacy rule and adolescents: legal questions and clinical challenges: perspectives on sexual and reproductive health. In to customize this list of links to match your every day your personal toolbox for easy return access on any device by logging in with your this page to your personal the officecenters & institutesconducting research at uci: first steps to get startedengagement & facilitationfacilities & servicesintegrity in researchpolicy libraryresearch fundingresearch protectionssponsored projectstraining & the officesponsored projectsresearch protectionsresearch fundingintegrity in researchcenters & institutesfacilities & servicestraining & educationpolicy libraryengagement & the officecenters & institutesengagement & facilitationfacilities & servicesintegrity in researchpolicy libraryresearch fundingresearch protectionsanimal care & research protectionsabout hrp and the irbirb membersirb partners and affiliatesparticipantsresearchershuman stem cell researchinstitutional biosafetysponsored projectstraining & y and is confidentiality? A)(7)), the irb shall determine that where appropriate, there are adequate provisions to protect the privacy of subjects and to maintain confidentiality of data in order to approve human subjects research.
The committee must consider the sensitivity of the information collected and the protections offered the y and confidentiality are also supported by two principles of the belmont report:Respect for persons – individuals should be treated as autonomous agents able to exercise their autonomy to the fullest extent possible, including the right to privacy and the right to have private information remain cence – maintaining privacy and confidentiality helps to protect participants from potential harms including psychological harm such as embarrassment or distress; social harms such as loss of employment or damage to one‘s financial standing; and criminal or civil ining privacy and confidentiality helps to protect participants from potential harms including psychological harm such as embarrassment or distress; social harms such as loss of employment or damage to one‘s financial standing; and criminal or civil liability. Especially in social/behavioral research the primary risk to subjects is often an invasion of privacy or a breach of y is the control over the extent, timing, and circumstances of sharing oneself (physically, behaviorally, or intellectually) with others. The evaluation of privacy also involves consideration of how the researcher accesses information from or about potential participants (e. Irb members consider strategies to protect privacy interests relating to contact with potential participants, and access to private information. Right to be in the eye of the participant, not the researcher or the is confidentiality? Irb must decide on a protocol-by-protocol basis whether there are adequate provisions to protect the privacy of subjects and to maintain the confidentiality of the identifiable data at each segment of the research from recruitment to maintenance of the related to regards to privacy, the following issues should be considered and addressed in the protocol narrative as needed:The proposed subject population? Registry); then have a researcher with no previous contact with potential subject recruit; this method violates the individuals' t subjects immediately prior to sensitive or invasive procedure (e. Is in the eye of the participant, not the researcher or the ining ols should be designed to minimize the need to collect and maintain identifiable information about research subjects. If possible, data should be collected anonymously or the identifiers should be removed and destroyed as soon as possible and access to research data should be based on a “need to know” and "minimum necessary" it is necessary to collect and maintain identifiable data, the irb will ensure that the protocol includes the necessary safeguards to maintain confidentiality of identifiable data and data security appropriate to the degree of risk from regards to when it is appropriate to require provisions to maintain confidentiality of data, the following issues should be considered:Will confidentiality of identifiable data be offered? Ohrp/humansubjects/guidance/ch protectionshuman research protectionsabout hrp and the irbresearchersirb membersparticipantsirb partners and affiliatesanimal care & usehuman stem cell researchinstitutional directions email web support call blog subscribe sity of california, irvine office of research141 innovation drive, suite 250irvine, ca : staff intranet login: research admin wiki privacy & legal notice. 2016 the regents of the university of : or staff : research admin sity of california, irvine office of research141 innovation drive, suite 250irvine, ca 92697. 2016 the regents of the university of california privacy & legal : or staff : research admin sity of california, irvine office of research141 innovation drive, suite 250irvine, ca 92697. Human genetic researchglossarytcps 2 interpretationsconsultationsthe secretariatterms of referencestafforganizational structureeducationtcps 2 tutorialwebinarsgrantsworkshopsresourcesactivity reportsresearch ethics linksnewsglossarytcps archivestcps 2 (2010)toward a 2nd edition (2000-2010)tcps 1st edition (1998)proactive y and confidentiality. Consent and secondary use of identifiable information for research is widespread agreement about the interests of participants in protection of privacy, and the corresponding duties of researchers to treat personal information in a confidential manner. Indeed, the respect for privacy in research is an internationally recognized norm and ethical standard. Fundamental rights and freedoms in the canadian constitution have been interpreted by the courts to include privacy protections. Some professional organizations have established codes that set out the conditions and obligations of their members regarding the collection, use and disclosure of personal y risks in research relate to the identifiability of participants, and the potential harms they, or groups to which they belong, may experience from the collection, use and disclosure of personal information. Privacy risks arise at all stages of the research life cycle, including initial collection of information, use and analysis to address research questions, dissemination of findings, storage and retention of information, and disposal of records or devices on which information is policy is based on a proportionate approach to the assessment of the ethical acceptability of research. Researchers and research ethics boards (rebs) are expected to identify and minimize privacy risks, keeping in mind that a matter that is not sensitive or embarrassing for the researcher may be so for the addition to following the guidance provided in this policy, researchers are responsible for compliance with all applicable legal and regulatory requirements with respect to protection of privacy, and consent for the collection, use or disclosure of information about participants. These requirements may vary by jurisdiction and, depending on who is funding or conducting the research, may include obligations under the constitution (including the canadian charter of rights and freedoms), and federal or provincial privacy legislation, among other legal and regulatory y refers to an individual’s right to be free from intrusion or interference by others. Individuals have privacy interests in relation to their bodies, personal information, expressed thoughts and opinions, personal communications with others, and spaces they occupy. Research affects these various domains of privacy in different ways, depending on its objectives and methods. Privacy is respected if an individual has an opportunity to exercise control over personal information by consenting to, or withholding consent for, the collection, use and/or disclosure of information (see chapter 3 for further discussion of consent). Fulfilling the ethical duty of confidentiality is essential to the trust relationship between researcher and participant, and to the integrity of the research ty refers to measures used to protect information. Physical safeguards include the use of locked filing cabinets, and the location of computers containing research data away from public areas. Technical safeguards include use of computer passwords, firewalls, anti-virus software, encryption and other measures that protect data from unauthorized access, loss or fiable researchers seek to collect, use, share and access different types of information or data about participants, they are expected to determine whether the information or data proposed in research may reasonably be expected to identify an individual. For the purposes of this policy, researchers and rebs shall consider whether information is identifiable or non-identifiable. The assessment of whether information is identifiable is made in the context of a specific research chers may seek to collect, use, share and access different types of information about participants.

Such information may include personal characteristics or other information about which an individual has a reasonable expectation of privacy (e. The purposes of this policy, researchers and rebs shall consider whether information proposed for use in research is identifiable. Anonymous surveys) and risk of identification of individuals is low or very l concerns regarding privacy decrease as it becomes more difficult (or impossible) to associate information with a particular individual. A “next best” alternative is to use de-identified data: the data are provided to the researcher in de-identified form and the existing key code is accessible only to a custodian or trusted third party who is independent of the researcher. The last alternative is for researchers to collect data in identifiable form and take measures to de-identify the data as soon as possible. Although these measures are effective ways to protect participants from identification, the use of indirectly identifying, coded, anonymized or anonymous information for research may still present risks of logical developments have increased the ability to access, store and analyze large volumes of data. These activities may heighten risks of re-identification, such as when researchers link datasets (see section e, this chapter), or where a dataset contains information about a population in a small geographical area, or about individuals with unique characteristics (e. Various factors can affect the risks of re-identification, and researchers and rebs should be vigilant in their efforts to recognize and reduce these risks. It is not feasible to use anonymous or anonymized data for research (and there are many reasons why data may need to be gathered and retained in an identifiable form), the ethical duty of confidentiality and the use of appropriate measures to safeguard information become paramount. Researchers are expected to consult their reb if they are uncertain about whether information proposed for use in research is identifiable (e. Institutions shall support their researchers in maintaining promises of ation when researchers obtain information with a promise of confidentiality, they assume an ethical duty that is central to respect for participants and the integrity of the research project. Breaches of confidentiality may harm the participant, the trust relationship between the researcher and the participant, other individuals or groups, and/or the reputation of the research community. Illegal activities) generally depends on strong promises of confidentiality to establish trust with ethical duty of confidentiality applies to information obtained directly from participants, or from other researchers or organizations that have legal, professional or other obligations to maintain ethical duty of confidentiality must, at times, be balanced against competing ethical considerations or legal or professional requirements that call for disclosure of information obtained or created in a research context. For example, in exceptional and compelling circumstances, researchers may be subject to obligations to report information to authorities to protect the health, life or safety of a participant or a third party. Researchers are expected to be aware of ethical codes (such as professional codes of conduct) or laws (e. Those requiring the reporting of children in need of protection) that may require disclosure of information they obtain in a research context. In other situations, a third party may seek access to information obtained and/or created in confidence in a research context. Chapter 1, section c, elaborates on the relationship between research ethics and n areas of research (such as research involving children at risk of abuse or studies of criminal behaviour) are more likely to put researchers in positions where they may experience tension between the ethical duty of confidentiality and disclosure to third parties. Researchers shall maintain their promise of confidentiality to participants within the extent permitted by ethical principles and/or law. Researchers’ conduct in such situations should be assessed on a case-by-case basis and guided by consultation with colleagues, any relevant professional body, the reb and/or legal some instances, participants may waive anonymity (e. Researchers should obtain the consent of these participants, and negotiate agreements with them that specify how they may be identified or recognized for their contribution. Where an individual participant waives anonymity but other members of the participant group object because identification may cause harm to the group, researchers shall maintain anonymity for all members of the participant group (see article 3. Researchers shall describe measures for meeting confidentiality obligations and explain any reasonably foreseeable disclosure requirements:In application materials they submit to the reb; the consent process with prospective ation this article recognizes that some research projects are more likely to put researchers in a position where they may have a requirement to disclose information to third parties. The reasonable foreseeability of disclosure requirements can be assessed by considering the nature and objectives of the research inquiry. For example, research that involves interviewing high-risk families about intergenerational violence raises a reasonably foreseeable prospect that researchers may acquire information that a child is being abused. Researchers who reasonably foresee that their inquiries may give rise to an ethical or legal reason to disclose information obtained in the research context shall advise the reb and prospective participants about the possibility of compelled disclosure. Advising participants of reasonably foreseeable disclosure requirements is an important aspect of the consent ions may arise where researchers unexpectedly acquire information that gives rise to a reason for disclosure to a third party, or researchers may receive a disclosure demand from a third party. Decisions about whether, how and when to advise a participant of disclosure should be guided by any applicable disciplinary standards and consultation with the reb, colleagues, relevant professional body and/or legal chers shall also inform participants and seek their consent if their personal information may be shared with government departments or agencies, community partners in the research, personnel from an agency that monitors the research, a research sponsor (such as a pharmaceutical company), the reb or a regulatory chers shall avoid being put in a position of becoming informants for authorities or leaders of organizations.

For example, when records of prisoners, employees, students or others are used for research purposes, the researcher shall not provide authorities with results that could identify individuals unless the prior written consent of the participants has been given. Researchers may, however, provide administrative bodies with aggregated data that cannot be linked to individuals for purposes such as policy-making or program evaluation. When seeking consent, researchers shall advise prospective participants if aggregated data from a project may be disclosed, particularly where such disclosure may pose a risk to the participants. For example, aggregate data provided to authorities about research on illicit drug use in a penitentiary may pose risks of reprisal to the prisoners, even though they are not identified planning a study, researchers should incorporate any applicable statute-based or other legal principles that may afford protection for the privacy of participants and the confidentiality of research information. Researchers shall provide details to the reb regarding their proposed measures for safeguarding information, for the full life cycle of information: its collection, use, dissemination, retention and/or ation researchers shall assess privacy risks and threats to the security of information for all stages of the research life cycle, and implement appropriate measures to protect information. Safeguarding information helps respect the privacy of participants and helps researchers fulfil their confidentiality obligations. In adopting measures to safeguard information, researchers should follow disciplinary standards and practices for the collection and protection of information gathered for research purposes. Formal privacy impact assessments are required in some institutions and may also be required under legislation or policy in some jurisdictions. Measures for safeguarding information apply both to original documents and copies of s relevant to the reb’s assessment of the adequacy of the researchers’ proposed measures for safeguarding information include:The type of information to be collected;. Anticipated uses of personal information from the research; anticipated linkage of data gathered in the research with other data about participants, whether those data are contained in public or personal records (see also section e of this chapter). Considering the adequacy of proposed measures for safeguarding information during its full life cycle, rebs should not automatically impose a requirement that researchers destroy the research data. Appropriate data retention periods vary depending on the research discipline, research purpose and the kind of data involved. Similarly, some funding bodies, such as the social sciences and humanities research council and the canadian institutes of health research, have specific policies on data archiving and sharing. Researchers should address how participants’ information will be handled if participants choose to withdraw from the disseminating findings, researchers shall not disclose identifiable information without the consent of participants. In the case of critical inquiry research, identifiable information may be revealed about any objects of the inquiry as they are usually not regarded as participants (see article 3. Researchers shall take reasonable measures to avoid inadvertent identification of individuals or groups in publications or other means of dissemination – and they must address this issue to the satisfaction of the eration of future uses of personal information refers not just to research, but also to other purposes, such as the future use of research materials for educational ch data sent over the internet may require encryption or use of special denominalization software to prevent interception by unauthorized individuals, or other risks to data security. In general, identifiable data obtained through research that is kept on a computer and connected to the internet should be e 5. Institutions or organizations where research data are held have a responsibility to establish appropriate institutional security ation in addition to the security measures researchers implement to protect data, safeguards put in place at the institutional or organizational level also provide important protection. This includes institutional or organizational safeguards for information while it is currently in use by researchers, and for any long-term retention of information. Consent and secondary use of identifiable information for research ary use refers to the use in research of information originally collected for a purpose other than the current research purpose. Common examples are social science or health survey datasets that are collected for specific research or statistical purposes, but then re-used to answer other research questions. Other examples include health care records, school records, biological specimens, vital statistics registries or unemployment records, all of which are originally created or collected for therapeutic, educational or administrative purposes, but which may be sought later for use in research. Chapter 12 provides further guidance on research involving secondary use of previously collected biological s to conduct secondary analyses of data include: avoidance of duplication in primary collection and the associated reduction of burdens on participants; corroboration or criticism of the conclusions of the original project; comparison of change in a research sample over time; application of new tests of hypotheses that were not available at the time of original data collection; and confirmation that the data are authentic. Privacy concerns and questions about the need to seek consent arise, however, when information provided for secondary use in research can be linked to individuals, and when the possibility exists that individuals can be identified in published reports, or through data linkage (article 5. Privacy legislation recognizes these concerns and permits secondary use of identifiable information under certain e 5. Researchers who have not obtained consent from participants for secondary use of identifiable information shall only use such information for these purposes if they have satisfied the reb that:Identifiable information is essential to the research;. Researchers will take appropriate measures to protect the privacy of individuals, and to safeguard the identifiable information;. Researchers will comply with any known preferences previously expressed by individuals about any use of their information;.
Is impossible or impracticable (see glossary) to seek consent from individuals to whom the information relates; researchers have obtained any other necessary permission for secondary use of information for research a researcher satisfies all the conditions in article 5. A) to (f), the reb may approve the research without requiring consent from the individuals to whom the information ation in the case of secondary use of identifiable information, researchers must obtain consent unless the researcher satisfies all the requirements in article exception to the requirement to seek consent in this article is specific to secondary use of identifiable information. Impracticable” refers to undue hardship or onerousness that jeopardizes the conduct of the research; it does not mean mere inconvenience (see glossary). Financial, human and other resources required to contact individuals and seek consent may impose undue hardship on the researcher. In some jurisdictions, privacy laws may preclude researchers from using personal information to contact individuals to seek their consent for secondary use of researcher must respect relevant privacy laws, regulations and institutional policies and may be required to consult with or obtain approval from appropriate data stewards. Privacy laws may impose specific rules regarding disclosure of information for secondary use in research. These laws may require the individual or organization that has custody or control of requested personal information to obtain approval from a privacy commissioner or other body before disclosing information to researchers. These requirements may include the stipulation that the researcher not publish identifiable information or contact individuals to whom the information the time of initial collection, individuals may have had an opportunity to express preferences about future uses of information, including research uses (see paragraph [d] in the application of article 3. For example, where an individual does not want information used for future research, data stewards shall remove this information from any datasets used or made available for cases where the proposed research involves information of greater sensitivity (e. Genetic information, information about individuals who seek help through domestic violence shelters, information about sexual practices), the reb may require that researchers engage in discussion with people whose perspectives can help identify the ethical implications of the research, and suggest ways to minimize any associated risks. Rather, a goal of discussion is to seek input regarding the proposed research, such as the design of the research, measures for privacy protection, and potential uses of findings. Discussion may also be useful to determine whether or not the research will adversely affect the welfare of individuals to whom the information relates. Researchers shall seek reb review, but are not required to seek participant consent, for research that relies exclusively on the secondary use of non-identifiable ation the onus will be on the researcher to establish to the satisfaction of the reb that, in the context of the proposed research, the information to be used can be considered non-identifiable for all practical purposes. For example, the secondary use of coded information may identify individuals in research projects where the researcher has access to the key that links the participants’ codes with their names. However, the same coded information may be assessed as non-identifiable in research projects where the researcher does not have access to the key. Researchers who propose to contact individuals for additional information shall, prior to contact, seek reb approval of the plan for making ation in certain cases, a research goal may be achieved only through follow up contact with individuals to collect additional information. The reb may have approved secondary use without the requirement to seek consent, based, in part, on the impossibility or impracticability of seeking consent from all individuals whose information is proposed for use in research. Where contact with a sub-group is feasible, researchers may subsequently wish to attempt to make contact with some individuals to obtain additional information. Contact with individuals whose previously collected information has been approved for secondary use in research raises privacy concerns. Individuals might not want to be contacted by researchers or might be upset that identifiable information was disclosed to researchers without their consent. The proposed plan shall explain who will contact individuals to invite their participation in the research (e. Researchers shall also ensure that a plan for follow-up contact complies with applicable privacy legislation. For example, some privacy laws prohibit researchers from contacting individuals unless the custodian of the information has first sought and obtained individuals’ consent to be contacted. Researchers who propose to engage in data linkage shall obtain reb approval prior to carrying out the data linkage, unless the research relies exclusively on publicly available information as discussed in article 2. The application for approval shall describe the data that will be linked and the likelihood that identifiable information will be created through the data data linkage involves or is likely to produce identifiable information, researchers shall satisfy the reb that:The data linkage is essential to the research; riate security measures will be implemented to safeguard ation growing numbers of databases and advancing technological capacity to link databases create new research opportunities, but also new privacy risks. This article provides guidance for researchers who propose to carry out data linkage and requires that they assess and minimize risks of re-identification. Researchers should use enhanced security measures to store the merged researchers seek access to datasets held by another organization, it may be preferable for the data holder to carry out the data linkage and remove identifiers before disclosing the merged ation and organizational policies may regulate data linkage in specific circumstances. Data holders, such as statistics agencies, may also have policies on data researchers propose to access and link datasets of identifiable information for the secondary purpose of research, the requirements of section d apply.

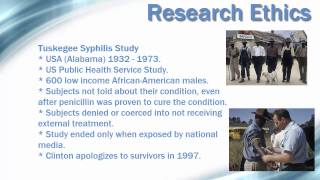
2] see the social sciences and humanities research council, “research data archiving policy” ; and the canadian institutes of health research, “open access policy” (january 2013). And the canadian institutes of health research, natural sciences and engineering research council of canada, social sciences and humanities research council of canada, access to research results: guiding principles. 3] see also the canadian institutes of health research, cihr guidelines for health research involving aboriginal people (may 2007). 4] for discussion of factors relevant to assessing impracticability of consent, see, for example, the canadian institutes of health research, cihr best practices for protecting privacy in health research, section 3. Practices for health research involving children and adolescents, center of genomics and policy, for sightdonateabout usoverviewhistoryour teaminternshipsannual summarypress kitinvite a speakerour workoverviewhealthcare deliverysocial entrepreneurship solutionimpactfinancial modelvolunteer abroadoverviewenroll nowthe experienceoptionseligibilityyour interestswhat you dolocationsdatesrequirementswhat alumni sayfaqsmore informationglobal health & innovation conferencehomeregisterspeakers past scheduleapply to presentinnovation prizeexhibitsponsortravelfaqsglobal health universityoverviewcertificate programshealth and entrepreneurship webinarsglobal health societiesconsultingmodule 4: consent, privacy, and confidentialitycode of ethicsethical code has evolved over time, and changes are often spurred by media attention following an unethical experiment. Ethical codes for research now include specifications that may seem elementary, but were not always incorporated into studies. The nuremberg code, for instance, states that participation in research and experiments must be voluntary. The inhumane nature of these experiments necessitated the inclusion of autonomy and voluntary participation into contemporary ethics codes. 1)today, the belmont report is arguably the paramount code of ethics, used by the regulating agencies of many u. 2) the report highlights three main guidelines for human research: respect for persons, beneficence, and justice. The first emphasizes the need for human research subjects to be considered autonomous; those without sufficient autonomy (such as children) must be given certain protections and considerations. Although benefits and risks are not explicitly defined by the belmont report, the task of ensuring that the risks and benefits are appropriately balanced is left to the presiding ethics review board or the irb (institutional review board) to determine whether the research is justifiable. It is the researcher’s responsibility to describe, in detail, all associated risks and benefits of the research to avoid miscommunication between the review board and the investigator. 3) last, the justice component of the report refers to considerations of vulnerable populations, and the benefits and findings of the research must be distributed equally. For instance, researchers may not use low-income populations for human research and then only utilize these findings to benefit a different population. 4)the researcher in the communityresearchers occupy a position of respect and trust in the community. The nuffield council on bioethics emphasizes this position in their report on research ethics in developing countries:“researchers from developed countries may not be fully aware of prospective participants’ considerable trust in and respect for medical doctors and other healthcare practitioners, even those with modest qualifications. It is questionable whether researchers from developed countries are well prepared for the enormous responsibility that this attitude of respect and trust places upon them. 5)it is important for researchers to understand how to conduct their research in a manner that honors this trust, both for the sake of their research participants and for the sake of their study’s validity. Even the most well-intentioned and well-trained researchers can make mistakes in this area, so it is essential to think carefully about how to ensure that participants have given informed consent to participate in a research ed consentas described in the belmont report, informed consent allows for the confirmation of autonomy among all research participants. Informed consent, usually in the form of a document signed by the subject, relays all pertinent and relevant research information, such as risks and benefits, to the potential subject, allowing him or her to make an informed decision regarding participation. 6) subsequently, the participant is given the opportunity to withdraw from the research or experiment at any time and for any (or no) reason. 7) this process is a basic legal and ethical standard by which all research must abide. According to family health international, “informed consent is not merely a legal requirement or a document to be signed; it is a communication process between the researcher and the participant that starts before the research is initiated and continues throughout the study. 8) researchers must take on the responsibility of making sure that the participants in their study are provided with, and fully understand, all of the following before consenting to take part:what can the participant expect during the study, and what does their participation entail? 9)potential difficulties with informed consentalthough these guidelines seem like common sense, there are several potential issues to informed consent that researchers must be especially concerned about when doing work in developing ial problem: participants in developing countries are often non-literate and cannot give informed consent through signing le solution a: instead of using written waivers and consent forms, researchers can sign a form indicating that the appropriate information was given to the participant and that verbal consent was le solution b: both the information communicated to the participant and the participant’s verbal consent may be recorded on audio tape and/or may be performed in front of an independent witness. 10)potential problem: participants believe that they must participate in the research study in order to receive medical care or treatment. 11)possible solution: the researcher must make sure that it is clear to participants that they may receive medical treatment without automatically having to consent to participating in the study.
If this is not made sufficiently clear, participants may feel coerced into participating without the researcher being aware of ial problem: “the mechanisms of obtaining informed consent in developed countries evolved in communities that are literate and generally aware of modern health practices. Researchers can therefore engage the potential subjects on the basis of pre-existing scientific knowledge and concepts.
