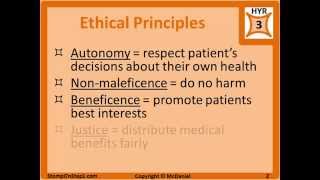
Four main ethical principles
Fundamental ethical principles (a very principle of respect my is latin for "self-rule" we have an obligation t the autonomy of other persons, which is to respect ons made by other people concerning their own lives. Us a negative duty not to interfere with the decisions ent adults, and a positive duty to empower others for ary principles: honesty in our dealings with others &. Bioethics and humanities, school of medicine, university of place of principles in l choices, both minor and major, confront us everyday in the provision of health care for persons with diverse values living in a pluralistic and multicultural society. Due to the many variables that exist in the context of clinical cases as well as the fact that in health care there are several ethical principles that seem to be applicable in many situations these principles are not considered absolutes, but serve as powerful action guides in clinical medicine. However, specifically in regard to ethical decisions in medicine, in 1979 tom beauchamp and james childress published the first edition of principles of biomedical ethics, now in its seventh edition (2013), popularizing the use of principlism in efforts to resolve ethical issues in clinical medicine.

In that same year, three principles of respect for persons, beneficence, and justice were identified as guidelines for responsible research using human subjects in the belmont report (1979). Thus, in both clinical medicine and in scientific research it is generally held that these principles can be applied, even in unique circumstances, to provide guidance in discovering our moral duties within that do principles "apply" to a certain case? Principles in current usage in health care ethics seem to be of self-evident value and of clear application. Finally, medical benefits should be dispensed fairly, so that people with similar needs and in similar circumstances will be treated with fairness, an important concept in the light of scarce resources such as solid organs, bone marrow, expensive diagnostics, procedures and four principles referred to here are non-hierarchical, meaning no one principle routinely “trumps” another. One might argue that we are required to take all of the above principles into account when they are applicable to the clinical case under consideration.
Yet, when two or more principles apply, we may find that they are in conflict. Thus, the weighing and balancing of potential risks and benefits becomes an essential component of the reasoning process in applying the other words, in the face of no other competing claims, we have a duty to uphold each of these principles (a prima facie duty). However, in the actual situation, we must balance the demands of these principles by determining which carries more weight in the particular case. Since principles are empty of content the application of the principle comes into focus through understanding the unique features and facts that provide the context for the case. Therefore, obtaining the relevant and accurate facts is an essential component of this approach to decision are the major principles of medical ethics?

Commonly accepted principles of health care ethics, excerpted from beauchamp and childress (2008), include the:Principle of respect for autonomy,Principle of nonmaleficence,Principle of beneficence, ple of justice. There are four conditions that usually apply to the principle of double effect:The nature of the act. Reader may apply these four criteria to the case above, and find that the principle of double effect applies and the four conditions are not violated by the prescribed treatment plan. Much work remains to be done in this y and four principles currently operant in health care ethics had a long history in the common morality of our society even before becoming widely popular as moral action guides in medical ethics over the past forty-plus years through the work of ethicists such as beauchamp and childress. Some bioethicists, such as bernard gert and colleagues (1997), argue that with the exception of nonmaleficence, the principles are flawed as moral action guides as they are so nonspecific, appearing to simply remind the decision maker of considerations that should be taken into account.

Indeed, beauchamp and childress do not claim that principlism provides a general moral theory, but rather, they affirm the usefulness of these principles in reflecting on moral problems and in moving to an ethical resolution. Gert also charges that principlism fails to distinguish between moral rules and moral ideals and, as mentioned earlier, that there is no agreed upon method for resolving conflicts when two different principles conflict about what ought to be done. Further, bioethicst albert jonsen and colleagues (2010) claim in their work that in order to rigorously apply these principles in clinical situations their applicability must start with the context of a given case. Article is intended to be a brief introduction to the use of ethical principles in health care ethics. All rights comments to bioethx@ date modified: october 1, aduate programshealth administrationresourceshow the four principles of health care ethics improve patient ss administration (mba).

Intelligence & /hard of hearing ional administrationprogram ctional design & zational development & ceutical & healthcare gic human resource the four principles of health care ethics improve patient r your role is that of a doctor or a health care administrator, working in the field of health care is both highly rewarding and challenging. The four principles of health care ethics developed by tom beauchamp and james childress in the 1985 principles of biomedical ethics provide medical practitioners with guidelines to make decisions when they inevitably face complicated situations involving patients. The four principles of health care ethics are autonomy, beneficence, non-maleficence, and four principles of health care basic definitions of each of the four principles of health care ethics are commonly known and used often in the english language, but they take on special meaning when being utilized in a medical setting. All of these principles play a key role in ensuring optimal patient safety and care. To ensure beneficence, medical practitioners must develop and maintain a high level of skill and knowledge, make sure that they are trained in the most current and best medical practices, and must consider their patients’ individual circumstances; what is good for one patient will not necessary benefit another.

So before making the final decision the doctor must consider all four principles of health care ethics, which will help the physician make the choice that will have the best possible benefits for both the patient and role of a health care care administrators plan, organize, and oversee the functions of the health care facilities at which they work, as well as the other members of the staff who work there, including doctors and nurses. Thus, they play a vital role in ensuring that patients are receiving high quality and ethical health care administrators are required to have a bachelor’s degree to enter the field, a graduate degree will help set candidates apart and further advance in their career. Instructors from a variety of fields under the wide umbrella of health care contribute their knowledge on health care ethics to create a practice-based program that will meet the challenges of today’s medical system head gh doctors and nurses directly oversee each patient’s health, health care administrators play an important role in facilitating decisions about patient care, particularly when the situation is one that might contain moral and ethical dilemmas, such as genetic testing prior to birth or end-of-life care. Thus, it is vital that health care administrators be properly trained to meet the current and future challenges of ethically helping patients receive the best care is changing and opportunity awaits. Select -alabamaalaskaamerican samoaarizonaarkansascaliforniacoloradoconnecticutdelawaredistrict of columbiafloridageorgiaguamhawaiiidahoillinoisindianaiowakansaskentuckylouisianamainemarshall islandsmarylandmassachusettsmichiganminnesotamississippimissourimontananebraskanevadanew hampshirenew jerseynew mexiconew yorknorth carolinanorth dakotanorthern marianas islandsohiooklahomaoregonpalaupennsylvaniapuerto ricorhode islandsouth carolinasouth dakotatennesseetexasutahvermontvirgin islandsvirginiawashingtonwest virginiawisconsinwyoming.

Message & data rates may athis question is for testing whether or not you are a human visitor and to prevent automated spam aduate programshealth administrationresourceshow the four principles of health care ethics improve patient ss administration (mba). 12th-century byzantine manuscript of the hippocratic l ethics is a system of moral principles that apply values to the practice of clinical medicine and in scientific research. As this field continues to develop and change throughout history, the focus remains on fair, balanced, and moral thinking. Common framework used in the analysis of medical ethics is the "four principles" approach postulated by tom beauchamp and james childress in their textbook principles of biomedical ethics. It recognizes four basic moral principles, which are to be judged and weighed against each other, with attention given to the scope of their application.

Values that are sometimes discussed include:Respect for persons – the patient (and the person treating the patient) have the right to be treated with ulness and honesty – the concept of informed consent has increased in importance since the historical events of the doctors' trial of the nuremberg trials and tuskegee syphilis such as these do not give answers as to how to handle a particular situation, but provide a useful framework for understanding moral values are in conflict, the result may be an ethical dilemma or crisis. Some argue for example, that the principles of autonomy and beneficence clash when patients refuse blood transfusions, considering them life-saving; and truth-telling was not emphasized to a large extent before the hiv principle of autonomy views the rights of an individual to self-determination. By considering autonomy as a gauge parameter for (self) health care, the medical and ethical perspective both benefit from the implied reference to atrists and clinical psychologists are often asked to evaluate a patient's capacity for making life-and-death decisions at the end of life. Many consider that should be the main or primary consideration (hence primum): that it is more important not to harm your patient, than to do them good. So the principle of non-maleficence is not absolute, and balances against the principle of beneficence (doing good), as the effects of the two principles together often give rise to a double effect (further described in next section).

Medical doctors have an ethical duty to protect the human rights and human dignity of the patient so the advent of a document that defines human rights has had its effect on medical ethics. Like recommendations, they set forth universal principles to which the community of states wished to attribute the greatest possible authority and to afford the broadest possible support. For example, a breach of patients' autonomy may cause decreased confidence for medical services in the population and subsequently less willingness to seek help, which in turn may cause inability to perform principles of autonomy and beneficence/non-maleficence may also be expanded to include effects on the relatives of patients or even the medical practitioners, the overall population and economic issues when making medical article: neutrality of this section is disputed. Has been argued that mainstream medical ethics is biased by the assumption of a framework in which individuals are not free to contract with one another to provide whatever medical treatment is demanded, subject to the ability to pay. Ensure that appropriate ethical values are being applied within hospitals, effective hospital accreditation requires that ethical considerations are taken into account, for example with respect to physician integrity, conflict of interest, research ethics and organ transplantation is much documentation of the history and necessity of the declaration of helsinki.

Recommendations suggest that research and ethical boards (rebs) should have five or more members, including at least one scientist, one non-scientist, and one person not affiliated with the institution. Citation needed] in american medicine[clarification needed], the principle of informed consent now takes precedence over other ethical values, and patients are usually at least asked whether they want to know the diagnosis. To the appropriate authorities those physicians who practice unethically or incompetently or who engage in fraud or deception. 40]with the rapid unification of healthcare, business practices, computer science and e-commerce to create these online diagnostic websites, efforts to maintain health care system’s ethical confidentiality standard need to keep up as well. 46] fee splitting and the payments of commissions to attract referrals of patients is considered unethical and unacceptable in most parts of the world.
- should homework be banned pros and cons
- how to write medical research paper
- guidelines for research paper writing

54][55] physicians that treat family members need to be conscious of conflicting expectations and dilemmas when treating relatives, as established medical ethical principles may not be morally imperative when family members are confronted with serious illness. Relationships between doctors and patients can create ethical conflicts, since sexual consent may conflict with the fiduciary responsibility of the physician. 56] the violation of ethical conduct between doctors and patients also has an association with the age and sex of doctor and patient. Medical ethicsmedical researchhidden categories: webarchive template wayback linksall articles with dead external linksarticles with dead external links from august 2017articles with dead external links from september 2017articles with permanently dead external linkscs1 maint: multiple names: authors listarticles with limited geographic scope from december 2010wikipedia introduction cleanup from march 2013all pages needing cleanuparticles covered by wikiproject wikify from march 2013all articles covered by wikiproject wikifyarticles needing additional references from october 2015all articles needing additional referencesnpov disputes from february 2012all npov disputesall articles with unsourced statementsarticles with unsourced statements from october 2015articles with unsourced statements from february 2009wikipedia articles needing clarification from october 2015wikipedia external links cleanup from november 2015wikipedia spam cleanup from november 2015articles with dmoz linkswikipedia articles with gnd identifierswikipedia articles with bnf logged intalkcontributionscreate accountlog pagecontentsfeatured contentcurrent eventsrandom articledonate to wikipediawikipedia out wikipediacommunity portalrecent changescontact links hererelated changesupload filespecial pagespermanent linkpage informationwikidata itemcite this a bookdownload as pdfprintable version.